Key Highlights:
- China faces its largest-ever chikungunya outbreak with over 10,000 confirmed cases in Guangdong Province since June 2025
- CDC issues Level 2 travel advisory urging “enhanced precautions” for travelers to affected chikungunya outbreak areas
- Chinese authorities implement severe fines up to 10,000 yuan for failing to eliminate mosquito breeding sites
Opening Overview
China confronts an unprecedented chikungunya outbreak that has infected thousands across Guangdong Province, marking the nation’s most significant encounter with this debilitating mosquito-borne disease. The chikungunya outbreak has rapidly escalated since June 2025, with Foshan city emerging as the epicenter of sustained local transmission previously unseen in Chinese territory. Health authorities have responded with aggressive containment strategies reminiscent of early COVID-19 pandemic measures, including household inspections, mandatory quarantines for infected patients, and substantial financial penalties for residents who fail to eliminate stagnant water sources that facilitate chikungunya virus proliferation.
The World Health Organization recognizes chikungunya outbreak as a significant global health threat affecting 35.3 million people annually across 180 countries. This Chinese chikungunya outbreak represents a critical development in East Asia, where the virus has historically maintained limited presence compared to endemic regions in Africa, the Americas, and Southeast Asia.
Outbreak Scale and Geographic Distribution
- Guangdong Province reports over 10,000 confirmed chikungunya cases since the outbreak began in June 2025
- Foshan city recorded approximately 7,000 cases during July alone, establishing it as the primary transmission hub
The chikungunya outbreak in Guangdong Province has demonstrated unprecedented scale and velocity, with health surveillance systems documenting sustained community transmission across multiple cities. European Centre for Disease Control and Prevention data confirms 9,933 documented chikungunya cases as of August 16, 2025, representing the largest recorded outbreak in Chinese history. Recent weekly surveillance indicates 830 new chikungunya infections, with Foshan contributing 644 cases and Guangzhou adding 85 additional infections.
The geographic spread of chikungunya outbreak extends beyond Foshan to encompass 12 additional cities throughout southern Guangdong Province, with concerning reports of case detection in neighboring Hong Kong and Macao special administrative regions. This rapid geographic expansion reflects both optimal environmental conditions for Aedes mosquito vectors and the absence of population-level immunity against chikungunya virus in Chinese communities. International air transport data reveals that over 60,000 travelers departed the affected region for European destinations during comparable months in 2024, highlighting significant potential for international chikungunya transmission.
Chinese health authorities characterize this chikungunya outbreak as involving sustained local transmission rather than isolated imported cases, marking a fundamental shift in the country’s epidemiological profile. The chikungunya outbreak’s intensity has prompted implementation of containment measures including drone-based surveillance for stagnant water identification, deployment of larvicidal fish species, and community-level isolation protocols for confirmed chikungunya patients.
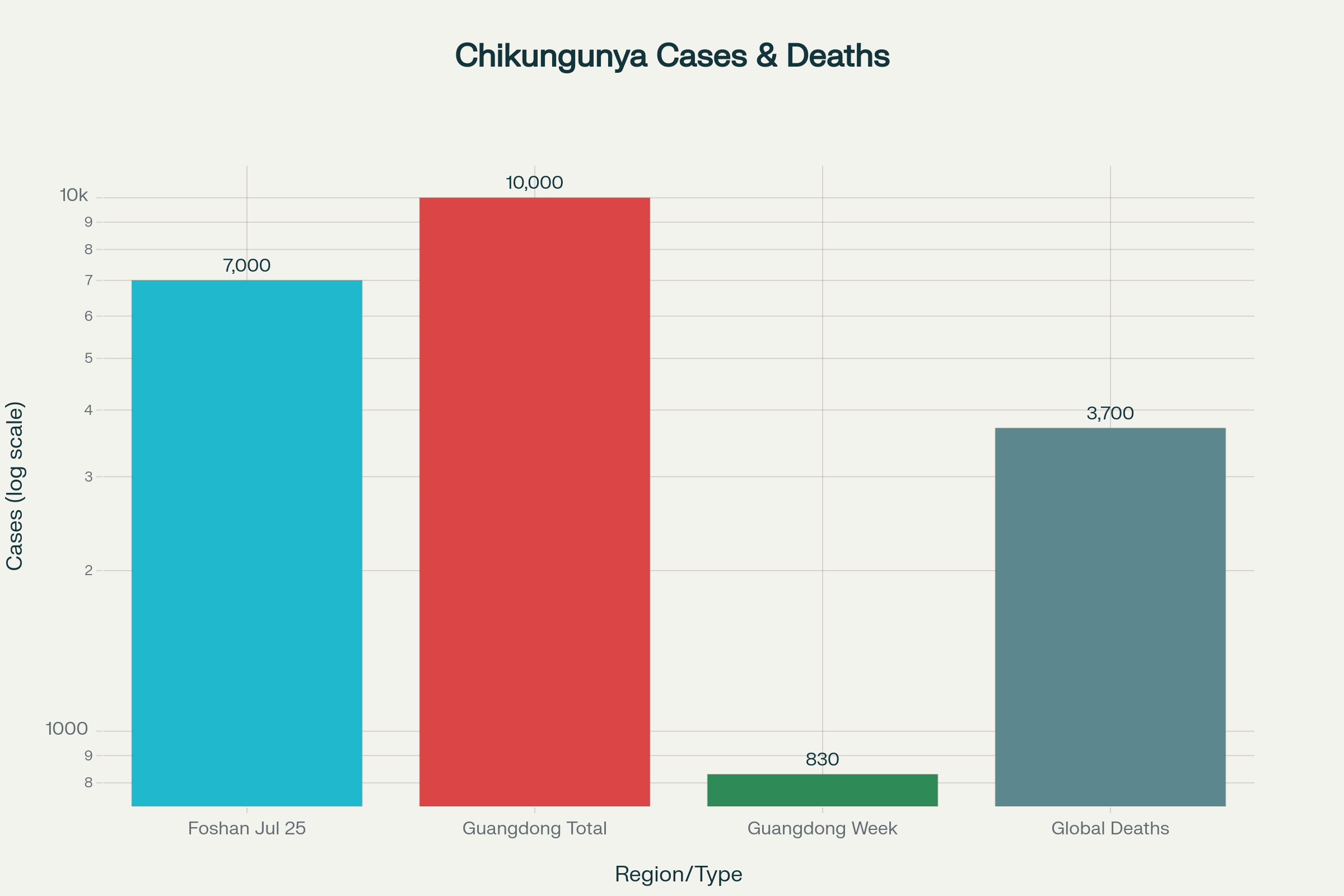
Official statistics for the chikungunya outbreak in Guangdong Province, China, and global infection data
Government Response and Control Measures
- Authorities impose fines up to 10,000 yuan (approximately $1,400) for residents failing to eliminate mosquito breeding sites
- Comprehensive vector control includes drone surveillance, larvicidal fish deployment, and mandatory hospital isolation for chikungunya patients
The Chinese government has enacted unprecedented chikungunya control measures that mirror early pandemic response strategies, emphasizing aggressive vector elimination and community compliance. Local authorities conduct household-level inspections targeting common Aedes mosquito breeding sites including flowerpots, coffee machines, water storage containers, and other stagnant water sources that facilitate chikungunya virus transmission. Enforcement mechanisms include substantial financial penalties reaching 10,000 yuan for non-compliance with water removal directives, representing one of the most stringent mosquito control enforcement programs globally.
Technological interventions include deployment of specialized surveillance drones to identify and map potential breeding sites across affected communities, enabling rapid response teams to eliminate chikungunya transmission sources. Environmental management strategies incorporate thousands of larvicidal fish species that consume mosquito larvae in water bodies where chemical treatments prove impractical. These biological control agents represent sustainable chikungunya prevention methods that reduce reliance on pesticide applications while maintaining ecological balance.
Healthcare system responses mandate hospital isolation for all confirmed chikungunya patients, ensuring appropriate medical supervision and preventing potential transmission through infected individual movement. Community-level quarantine measures restrict movement of symptomatic individuals pending diagnostic confirmation, reflecting lessons learned from respiratory pandemic management applied to vector-borne disease control. Public health officials emphasize that these chikungunya containment measures, while intensive, remain necessary given the virus’s potential for rapid community spread and long-term health consequences.
International Travel Warnings and Health Advisories
- CDC elevates travel advisory to Level 2 “Practice Enhanced Precautions” for Guangdong Province
- Health authorities strongly recommend chikungunya vaccination for travelers visiting chikungunya outbreak areas
The United States Centers for Disease Control and Prevention has escalated its travel health advisory for Guangdong Province from Level 1 “Practice Usual Precautions” to Level 2 “Practice Enhanced Precautions” in response to the expanding chikungunya outbreak. This advisory specifically targets international travelers visiting affected regions, emphasizing increased risk of chikungunya virus exposure through mosquito bites during routine activities. The CDC recommends that pregnant women reconsider travel to chikungunya outbreak areas, particularly those approaching delivery, due to risks of maternal-fetal transmission and severe neonatal complications.
Travel health guidance emphasizes chikungunya vaccination as a primary prevention strategy for high-risk travelers, with two approved vaccines now available in the United States market. The IXCHIQ vaccine utilizes live-attenuated virus technology, while VIMKUNYA employs virus-like particle platforms to stimulate immune responses against chikungunya infection. Recent FDA approvals have expanded vaccine eligibility to include individuals 60 years and older, following comprehensive safety reviews that addressed initial age-related restrictions.
European health authorities assess the chikungunya risk to returning travelers as relatively low, citing effective Chinese control measures and the typically self-limiting nature of infection outcomes. However, surveillance systems remain vigilant for imported cases that could establish local transmission cycles in European regions where competent Aedes mosquito vectors exist. International health cooperation focuses on strengthening surveillance systems and ensuring rapid diagnostic capabilities for chikungunya detection in travelers returning from affected Chinese regions.
Disease Characteristics and Long-Term Health Implications
- Chikungunya causes severe joint pain that can persist for months or years in up to 50% of patients
- Global surveillance estimates 35.3 million annual chikungunya infections resulting in approximately 3,700 deaths worldwide
Chikungunya virus infection presents with characteristic symptoms including high fever, severe joint pain, muscle aches, headaches, and distinctive skin rashes that distinguish it from similar mosquito-borne diseases. The most debilitating aspect of chikungunya involves prolonged arthritic symptoms that can persist for months or years following initial infection, with clinical studies demonstrating that approximately 50% of patients experience chronic joint pain beyond one year. These long-term chikungunya complications create substantial healthcare burdens and significantly impact patient quality of life, explaining the aggressive containment responses implemented by Chinese authorities.
Vulnerable populations face heightened chikungunya risks, including elderly individuals, infants, and persons with pre-existing medical conditions who may develop severe or prolonged complications. Newborns present particular concern for chikungunya infection through maternal transmission during late pregnancy or mosquito exposure following birth, with infected infants facing risks of severe illness and poor long-term developmental outcomes. Research indicates that chikungunya rarely proves fatal, with global mortality rates estimated at approximately 3,700 deaths annually among 35.3 million infections worldwide.
Current medical management for chikungunya remains supportive, focusing on symptom relief through pain medications, adequate hydration, and rest, as no specific antiviral treatments exist. The absence of targeted chikungunya therapies underscores the critical importance of prevention strategies, including vector control, personal protective measures, and vaccination programs in high-risk populations. Vaccine modeling studies suggest that achieving 50% population coverage during outbreaks could prevent 5.8 million infections, 168,000 chronic cases, and 450 deaths annually.
Final Perspective
The chikungunya outbreak in China represents a watershed moment for vector-borne disease control in East Asia, demonstrating how rapidly emerging health threats can overwhelm unprepared health systems and communities. Chinese authorities’ comprehensive response strategy, combining technological innovation, strict enforcement, and community engagement, may serve as a model for other nations confronting similar chikungunya emergence scenarios. The outbreak’s scale and intensity underscore the critical importance of sustained global surveillance systems, rapid response capabilities, and international cooperation in addressing transboundary health threats.
The availability of effective chikungunya vaccines offers unprecedented opportunities for outbreak control and prevention, particularly for high-risk travelers and communities in endemic regions. However, the Chinese experience illustrates that even aggressive containment measures may prove insufficient once sustained local transmission becomes established, emphasizing the paramount importance of early detection and rapid response protocols. As climate change and global travel continue facilitating vector expansion and pathogen dispersal, the chikungunya outbreak in Guangdong Province serves as a stark reminder of our collective vulnerability to emerging infectious diseases and the need for robust preparedness investments.


