Key Highlights:
- Six human rabies deaths occurred in the past 12 months, marking the highest annual toll in years according to CDC surveillance
- Federal officials are actively monitoring 15 rabies outbreaks spanning from New York to Oregon, affecting multiple wildlife species
- Pet vaccine hesitancy threatens to expand transmission risk from wildlife to domestic animals, with 40% of Americans believing canine vaccines are unsafe
Opening Overview: Peak Season Brings Unprecedented Surge
The United States is experiencing its most significant rabies outbreaks activity in years, with federal health officials tracking 15 distinct hotspots across the nation during what experts call peak rabies season. The Centers for Disease Control and Prevention reports six human fatalities from rabies in the past 12 months, representing the highest annual death toll recorded in several years. This alarming surge in rabies cases coincides with widespread wildlife infections affecting everything from skunks in Kentucky to gray foxes in Arizona, creating an urgent public health scenario that demands immediate attention.
'There are parts of the U.S. where it does seem like we’re getting more calls and more reports': Six deaths from rabies have been reported over the last 12 months in the U.S., the highest number in years, according to the CDC. https://t.co/Nn4i4n3aYk
— AVMA (American Veterinary Medical Association) (@AVMAvets) September 2, 2025
Dr. Ryan Wallace, who leads the CDC‘s rabies team, confirms the agency is “currently tracking 15 different likely outbreaks” spanning multiple states including Nassau County, New York, Cape Cod, Massachusetts, and regions across Alaska, Arizona, California, Indiana, Kentucky, Maine, North Carolina, Oregon, and Vermont. The comprehensive surveillance data reveals that rabies outbreaks are becoming increasingly common as shrinking natural habitats force wildlife into closer contact with human populations.
The escalating rabies situation represents a critical shift from historical patterns, with wildlife infections driving the majority of new cases while pet vaccination hesitancy threatens to compound the problem.
Wildlife Habitat Loss Drives Geographic Expansion of rabies Outbreaks
Wildlife populations across the United States are experiencing unprecedented rabies transmission rates, with multiple species serving as vectors for the deadly virus. The CDC surveillance system documents that bats remain the primary source of rabies infections in humans while simultaneously being the species most frequently infected with the virus. Current monitoring reveals rabies outbreaks affecting raccoons on Long Island, skunks throughout Kentucky, and gray foxes in Arizona, demonstrating the geographic diversity of affected wildlife populations.
Franklin County, North Carolina exemplifies the dramatic increase in rabies cases, with confirmed infections in wild animals doubling over the past year despite the rabies season remaining incomplete. County Health Director Scott LaVigne attributes this 100% spike in rabies cases to rapid urban development, noting that Franklin County’s population has increased 35% since 2010, forcing wildlife into increasingly dense concentrations where rabies transmission accelerates significantly.
The correlation between habitat loss and rabies outbreaks becomes evident when examining development patterns across affected regions. New housing developments and commercial expansion reduce available wilderness areas, creating conditions where previously isolated animal populations converge in smaller spaces, facilitating rapid virus transmission among wildlife communities that historically maintained natural separation.
Urban encroachment fundamentally alters wildlife behavior patterns, with animals displaying unusual characteristics that increase human exposure risk during rabies outbreaks.
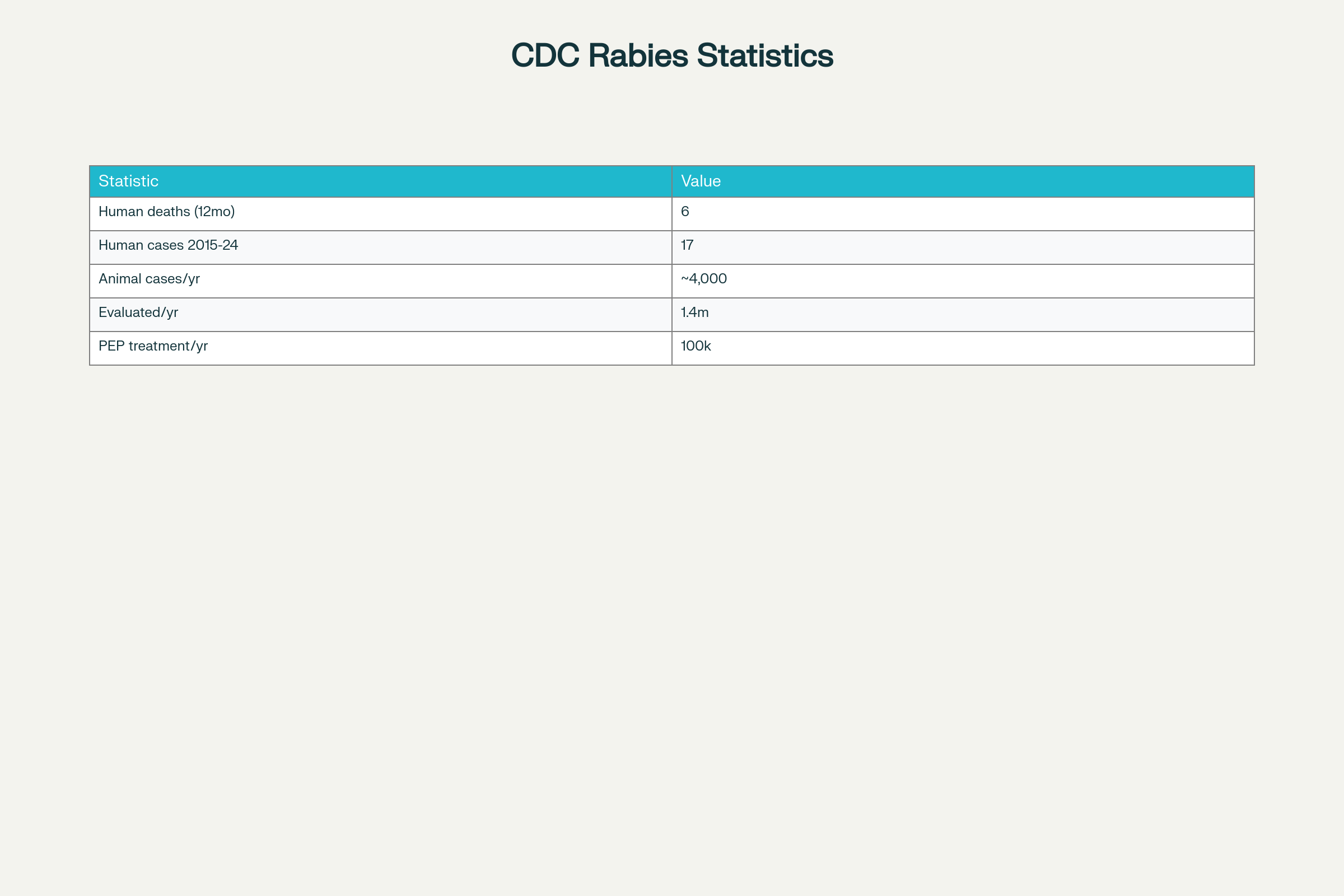
CDC Official Rabies Data Points in the US
Human Exposure Patterns Reveal Critical Detection Challenges
Current surveillance data reveals that approximately 1.4 million Americans undergo evaluation for potential rabies exposure annually, with 100,000 individuals receiving post-exposure prophylaxis to prevent infection. These statistics underscore the widespread nature of human-animal interactions that could potentially result in rabies transmission, particularly during outbreak periods when infected wildlife behavior becomes increasingly unpredictable.
Recent cases demonstrate how rabies exposure can occur without obvious symptoms or clear awareness of contact. Samantha Lang’s experience in Greenwood, Indiana illustrates typical exposure scenarios, where a bat entering her apartment through a ceiling hole resulted in tiny bite marks that initially went unnoticed. The discovery of the living bat hanging from her air conditioning vent prompted immediate medical consultation and post-exposure prophylaxis, highlighting how rabies cases often involve subtle initial contact.
Health officials emphasize that rabies virus can manifest differently depending on animal species and viral strain, with some infected animals displaying docile, friendly behavior rather than expected aggressive symptoms. Franklin County’s recent case involving a family that petted and fed a seemingly friendly raccoon demonstrates this dangerous misconception, where the animal’s attractive demeanor masked lethal rabies infection that required emergency vaccination for all family members following post-mortem testing.
The challenge of recognizing rabies outbreaks exposure becomes particularly acute with bat encounters, where bite marks may be minimal and easily overlooked, yet the virus transmission risk remains extremely high during outbreak conditions.
Vaccine Hesitancy Threatens Domestic Animal Protection Barriers
Pet vaccination rates face unprecedented challenges as vaccine hesitancy spreads among American pet owners, creating potential pathways for rabies transmission from wildlife to domestic animals. Research published in the journal Vaccine reveals that nearly 40% of Americans believe canine vaccines are unsafe, while 37% fear that vaccines could cause cognitive issues such as autism in their pets. These concerning attitudes threaten to undermine decades of successful rabies prevention efforts that eliminated canine rabies strains from the United States.
Dr. Gabriella Motta, a veterinarian from Glenolden, Pennsylvania and co-author of the vaccination study, reports frequent encounters with clients concerned about vaccine safety for their pets. The veterinary community expresses growing alarm about potential consequences if vaccination rates continue declining, particularly as rabies outbreaks expand throughout wildlife populations across multiple states.
Historical context demonstrates the critical importance of consistent pet vaccination programs, with domestic animals representing the primary source of human rabies infections prior to the 1960s. The successful elimination of canine rabies strains through strict vaccination laws and consistent immunization programs created the current protection barrier that prevents wildlife rabies from spreading to household pets and subsequently to human populations.
Current rabies outbreaks conditions amplify the urgency of maintaining high pet vaccination rates, as infected wildlife increasingly encounters domestic animals in suburban and urban environments where habitat boundaries continue shrinking.
Medical Response Evolution Enhances Treatment Accessibility
Modern rabies treatment protocols have evolved significantly from historical methods, with current post-exposure prophylaxis involving an immediate immunoglobulin injection containing rabies antibodies, followed by four vaccine doses administered in the arm rather than the abdomen. This streamlined approach maintains nearly 100% effectiveness when administered promptly after exposure, providing reliable protection during the current rabies outbreaks surge affecting multiple regions.
The CDC’s National Rabies Surveillance System continues tracking approximately 4,000 animal rabies cases annually, with over 90% occurring in wildlife species including bats, raccoons, skunks, and foxes. This comprehensive monitoring enables rapid response to emerging rabies outbreaks while supporting the medical infrastructure required to treat the 100,000 Americans who receive post-exposure prophylaxis each year.
Advanced surveillance capabilities allow health officials to identify rabies outbreaks patterns before human transmission occurs, as demonstrated in Nassau County, New York, where authorities declared an “imminent public health threat” after detecting 25 rabid animals, primarily raccoons and feral cats. Early detection systems combined with improved treatment accessibility create multiple protection layers against rabies transmission during peak outbreak periods.
The integration of veterinary and human health surveillance systems ensures coordinated responses that address both wildlife rabies sources and human exposure risks simultaneously across affected regions.
Final Assessment: Coordinated Response Essential for Outbreak Control
The current rabies outbreaks surge across 15 states represents the most significant public health challenge from this deadly virus in years, requiring immediate coordinated action from health officials, veterinarians, and communities. With six human deaths in the past 12 months compared to 17 total cases from 2015-2024, the acceleration in rabies fatalities demands heightened awareness and preventive measures across all affected regions. The combination of wildlife habitat loss, expanding urban development, and concerning vaccine hesitancy trends creates a complex challenge that transcends traditional rabies control methods.
Federal and state surveillance systems provide essential early warning capabilities, but success in controlling these rabies outbreaks depends critically on maintaining high pet vaccination rates and public education about exposure risks. The CDC’s tracking of 15 active outbreak areas demonstrates both the scope of the current crisis and the robust monitoring capabilities available to guide response efforts. As peak rabies season continues, the emphasis must remain on protecting both wildlife corridors and human communities through science-based prevention strategies that address the underlying causes driving this unprecedented surge in rabies transmission.


