Key Highlights
- One in six bacterial infections worldwide now resist standard antibiotic treatments, with WHO antibiotic resistance data showing resistance rising 5-15% annually across 40% of monitored pathogen-antibiotic combinations
- India faces severe antimicrobial resistance with over 297,000 deaths directly attributable to resistant bacteria annually, representing 30% of global AMR deaths in South Asia according to WHO antibiotic resistance surveillance
- Carbapenem resistance in Indian hospitals has reached alarming levels, with 88% resistance in Acinetobacter baumannii and 58% in Klebsiella pneumoniae by 2023
Initial Context
The World Health Organization’s October 2025 Global WHO Antibiotic Resistance Surveillance Report has delivered an unprecedented warning about the escalating global crisis of antimicrobial resistance. Drawing data from over 23 million bacteriologically confirmed cases across 104 countries, the WHO antibiotic resistance findings reveal that antibiotic resistance has reached critical levels worldwide, with India emerging as one of the most vulnerable nations to this growing threat.
The WHO’s Global Antimicrobial Resistance and Use Surveillance System (GLASS) data demonstrates that WHO antibiotic resistance increased in over 40% of the pathogen-antibiotic combinations monitored between 2018 and 2023, with an average annual increase of 5-15%. This represents the first comprehensive global analysis of its kind, providing crucial insights into the scope and trajectory of WHO antibiotic resistance patterns across different regions and healthcare systems.
For India, these WHO antibiotic resistance statistics paint a particularly concerning picture. The country confronts multiple overlapping factors that amplify its vulnerability to antibiotic resistance, including high infectious disease burden, widespread antibiotic misuse, and systemic healthcare challenges. With antimicrobial resistance contributing to over 1.04 million deaths annually in India, the nation stands at the epicenter of a public health emergency that threatens to undermine decades of medical progress.
Regional Variations in Resistance Patterns
The WHO antibiotic resistance report reveals significant geographical disparities in antibiotic resistance rates globally. The South-East Asian and Eastern Mediterranean regions, where India is positioned, show the highest WHO antibiotic resistance levels, with approximately one in three infections demonstrating antibiotic resistance compared to the global average of one in six. This regional concentration highlights the urgent need for targeted interventions in areas with weaker healthcare infrastructure and limited diagnostic capabilities.
European and Western Pacific regions demonstrate significantly lower WHO antibiotic resistance rates, with some areas showing resistance levels three times lower than those observed in South-East Asia. These variations underscore the critical importance of healthcare system strength, antibiotic stewardship programs, and comprehensive surveillance networks in controlling WHO antibiotic resistance spread.
India’s Alarming Antimicrobial Resistance Statistics
India’s WHO antibiotic resistance landscape presents one of the most challenging scenarios globally, with multiple factors converging to create a perfect storm for resistant pathogen proliferation. According to the Indian Council of Medical Research’s 2023 surveillance data, the country processed 99,492 culture-positive isolates, revealing deeply concerning WHO antibiotic resistance trends across major bacterial pathogens.
The ICMR’s Antimicrobial Resistance Surveillance Network data shows that Escherichia coli susceptibility to carbapenems has declined dramatically from 81.4% in 2017 to 62.7% in 2023 for imipenem, while meropenem susceptibility dropped from 73.2% to 66.0% over the same period. Similarly, Klebsiella pneumoniae demonstrates even more severe WHO antibiotic resistance patterns, with carbapenem susceptibility falling from 58.5% to 35.6% for imipenem and from 48% to 37.6% for meropenem between 2017 and 2023.
Critical Pathogen Resistance Levels
Among the most concerning developments is the emergence of extensively drug-resistant pathogens in Indian healthcare facilities. Acinetobacter baumannii, a leading cause of hospital-acquired infections, demonstrates 88% resistance to carbapenems according to 2023 ICMR data tracking WHO antibiotic resistance. This pathogen has become particularly problematic in intensive care units, where it frequently causes ventilator-associated pneumonia with limited treatment options remaining.
Pseudomonas aeruginosa resistance has shown a gradual but steady increase, with WHO antibiotic resistance rising from 26% in 2017 to 38.5% in 2023 for imipenem. Over 50% of carbapenem-resistant Pseudomonas aeruginosa isolates harbor metallo-β-lactamase enzymes, with NDM being the most common variant, severely limiting therapeutic options for infected patients.
Healthcare-Associated Infection Burden
The healthcare-associated infection data from India reveals the critical impact of WHO antibiotic resistance on patient outcomes. Among central line-associated bloodstream infections (CLABSI), 73.6% are caused by Gram-negative organisms, with 80% of Klebsiella pneumoniae and 91% of Acinetobacter baumannii isolates showing imipenem resistance. These WHO antibiotic resistance statistics demonstrate how antibiotic resistance has transformed routine medical procedures into high-risk interventions.
The prevalence of methicillin-resistant Staphylococcus aureus (MRSA) has increased from 33% in 2017 to 44.5% in 2023, while vancomycin resistance in Enterococcus species has risen to 17.5%, with E. faecium showing five times higher WHO antibiotic resistance rates than E. faecalis. These trends indicate that even traditionally effective antibiotics are losing their therapeutic value across multiple pathogen groups.
🚨Drug-resistant bacteria are becoming more dangerous worldwide.
— World Health Organization (WHO) (@WHO) October 14, 2025
Life-saving antibiotics are losing effectiveness, increasing infection risks and limiting treatment options.
Some resistant infections can only be treated with antibiotics that are costly, difficult to access, and… pic.twitter.com/oBucARiMYC
Economic and Public Health Impact Assessment
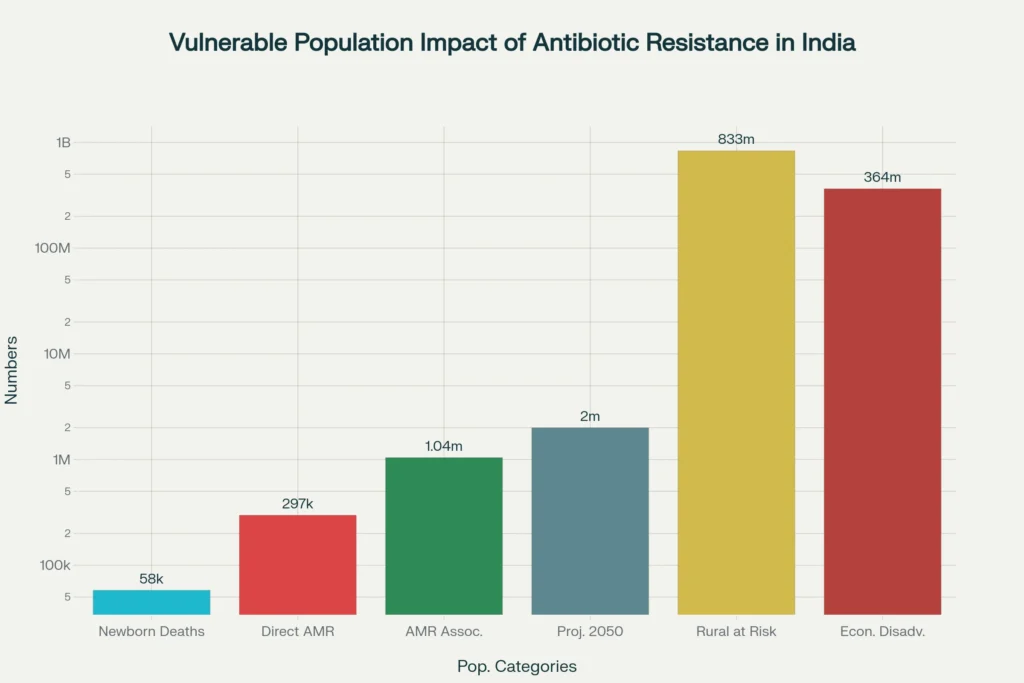
The economic burden of WHO antibiotic resistance in India extends far beyond direct healthcare costs, encompassing broader societal impacts that threaten the country’s development trajectory. Research indicates that India accounts for approximately 30% of antimicrobial resistance-related deaths in South Asia, with direct mortality figures reaching 297,000 annually and contributing factors in over 1.042 million additional deaths.
Healthcare systems face unprecedented challenges as routine infections become difficult-to-treat conditions requiring expensive, prolonged interventions. Patients with resistant infections experience longer hospital stays, higher mortality rates, and increased healthcare costs, while healthcare providers struggle with limited therapeutic options. The cascade effect impacts surgical procedures, cancer treatments, and organ transplantations that depend on effective antibiotic prophylaxis.
Vulnerable Population Impact
Rural and economically disadvantaged populations bear disproportionate burdens from WHO antibiotic resistance due to limited access to quality healthcare and diagnostic services. The WHO report emphasizes that communities with reduced access to proper diagnostics and care are more vulnerable to resistance consequences. In India’s context, this creates a dual challenge where populations most at risk have the least access to alternative treatment options when first-line antibiotics fail.
Children represent a particularly vulnerable demographic, with over 58,000 newborns dying annually from sepsis caused by resistant bacteria, a figure projected to reach 2 million deaths by 2050 if current WHO antibiotic resistance trends continue. This pediatric impact threatens India’s demographic dividend and long-term human development goals.
Surveillance and Response Mechanisms
India’s response to the WHO antibiotic resistance crisis centers on the Indian Council of Medical Research’s Antimicrobial Resistance Surveillance Network (AMRSN), established in 2013 to monitor resistance patterns across key pathogenic groups. The network operates through tertiary care hospitals, providing critical data on WHO antibiotic resistance trends while acknowledging limitations in community-level representation.
The AMRSN’s 2023 report analyzed 99,492 culture-positive isolates across multiple specimen types, generating comprehensive data on WHO antibiotic resistance patterns, mechanisms, and geographical distributions. However, significant gaps remain in surveillance coverage, particularly in rural areas and community settings where antibiotic use patterns may differ substantially from hospital environments.
Laboratory Network Expansion
India’s laboratory network for WHO antibiotic resistance surveillance has expanded significantly, with trained facilities conducting antibiotic susceptibility testing using standardized methodologies including broth microdilution and agar dilution techniques. The network contributes data to WHO’s GLASS system, supporting global WHO antibiotic resistance surveillance efforts while informing national policy decisions.
Regional centers across India demonstrate varying WHO antibiotic resistance patterns, with some facilities reporting higher percentages of specific pathogens and resistance mechanisms. This geographical variation highlights the need for tailored intervention strategies that account for local epidemiological patterns and healthcare infrastructure capabilities.
Policy Implementation Challenges
Despite having a National Action Plan on Antimicrobial Resistance launched in 2017, implementation across states remains uneven due to financial constraints, coordination challenges, and enforcement limitations. The policy framework emphasizes One Health approaches integrating human, animal, and environmental health considerations, but practical implementation faces significant obstacles in resource allocation and inter-sectoral coordination.
Strategic Interventions and Future Outlook
Addressing India’s WHO antibiotic resistance crisis requires comprehensive, multi-sectoral interventions that tackle both supply-side and demand-side factors contributing to resistance development. The WHO’s recommendations emphasize strengthening surveillance systems, improving diagnostic capabilities, and implementing robust antibiotic stewardship programs across healthcare settings.
Healthcare provider education and awareness programs represent critical components of WHO antibiotic resistance control strategies. Current data suggests significant knowledge gaps among prescribers regarding appropriate antibiotic selection, dosing, and duration, contributing to suboptimal prescribing practices that fuel resistance development. Standardized treatment guidelines and clinical decision support systems could help improve prescribing behaviors across different healthcare levels.
Innovation and Alternative Approaches
India’s pharmaceutical sector has begun developing indigenous antibiotic options, with recent approvals of drugs like Nafithromycin representing important steps toward reducing dependence on traditional antibiotics. However, the pipeline for new antibiotic development remains insufficient to match the pace of WHO antibiotic resistance emergence, necessitating greater investment in research and development activities.
Non-antibiotic approaches including vaccination programs, infection prevention measures, and improved sanitation infrastructure offer complementary strategies for reducing antibiotic demand. Enhanced hygiene practices, particularly in healthcare settings, can significantly reduce infection transmission and subsequent antibiotic requirements.
Global Cooperation Requirements
The transnational nature of WHO antibiotic resistance demands coordinated international responses that recognize the interconnectedness of global health security. Resistant pathogens cross borders through travel, trade, and migration, making unilateral national approaches insufficient for controlling WHO antibiotic resistance spread. India’s participation in global surveillance networks and collaborative research initiatives represents essential components of effective resistance management.
Technology transfer and capacity building programs can help strengthen surveillance and diagnostic capabilities in resource-limited settings, while international funding mechanisms could support infrastructure development and training programs necessary for comprehensive WHO antibiotic resistance control efforts.
Closing Assessment
The WHO’s 2025 Global WHO Antibiotic Resistance Surveillance Report represents a watershed moment in understanding the scope and urgency of the antimicrobial resistance crisis confronting global health systems. For India, the data reveals a nation at the epicenter of a public health emergency that threatens to undermine medical advances and jeopardize population health outcomes across multiple demographic groups.
With one in six bacterial infections worldwide now resistant to standard antibiotic treatments, and WHO antibiotic resistance rates in South-East Asia reaching one in three infections, the window for effective intervention is rapidly narrowing. India’s specific vulnerabilities, including high infectious disease burden, widespread antibiotic misuse, and systematic healthcare challenges, position the country as both a critical battleground and a potential catalyst for global WHO antibiotic resistance control efforts.
The path forward requires unprecedented coordination across government agencies, healthcare systems, pharmaceutical industries, and civil society organizations. Success in controlling WHO antibiotic resistance will determine not only India’s health security but also its contribution to global efforts to preserve antibiotic effectiveness for future generations. The time for incremental responses has passed; only comprehensive, sustained action can address the magnitude of this crisis and protect the foundation of modern medical practice.


