Key Highlights:
- WHO’s second Global Hypertension Report shows 1.4 billion people lived with hypertension in 2024, yet only one in five have it under control
- Cardiovascular diseases including hypertension are projected to cost low and middle-income countries US$3.7 trillion between 2011-2025
- Analysis of 195 countries reveals 99 nations have national hypertension control rates below 20 percent
The global hypertension crisis continues to deepen as the World Health Organization’s latest report exposes alarming gaps in blood pressure management worldwide. With over 1000 lives lost hourly to strokes and heart attacks caused by high blood pressure, this health emergency represents one of the most pressing public health challenges of our time. The WHO’s second Global Hypertension Report, released during the UN General Assembly in New York, reveals that despite hypertension being both preventable and treatable, the global hypertension crisis persists as most affected individuals lack adequate control. This escalating situation demands immediate international attention as millions face preventable deaths and countries confront mounting economic losses.
New WHO report finds 1.4 billion people live with #hypertension.
— World Health Organization (WHO) (@WHO) September 23, 2025
Hypertension is the number one risk factor for:
‼️ Heart attack
‼️ Stroke
and can lead to:
‼️ Chronic kidney disease
‼️ Dementia
Get your blood pressure checked today! Learn more 👉https://t.co/rO4S68pJ6r… pic.twitter.com/phFXVULP9j
Staggering Statistics Highlight Worldwide Treatment Gaps
- 1.4 billion people worldwide lived with hypertension in 2024, representing the largest affected population in recorded history
- Only 28% of low-income countries report general availability of all WHO-recommended hypertension medicines
- 99 out of 195 countries analyzed show national hypertension control rates below 20 percent
The scope of the global hypertension crisis becomes clear through WHO’s comprehensive analysis of 195 countries and territories. Current data reveals that despite affecting 1.4 billion individuals globally, this condition remains largely uncontrolled, with just over one in five patients achieving proper blood pressure management through medication or lifestyle modifications.

The global hypertension crisis disproportionately impacts low and middle-income nations, where only 54% of adults with hypertension receive proper diagnosis, 42% obtain treatment, and merely 21% achieve adequate control. These statistics underscore how this health emergency perpetuates health inequalities across different economic regions.
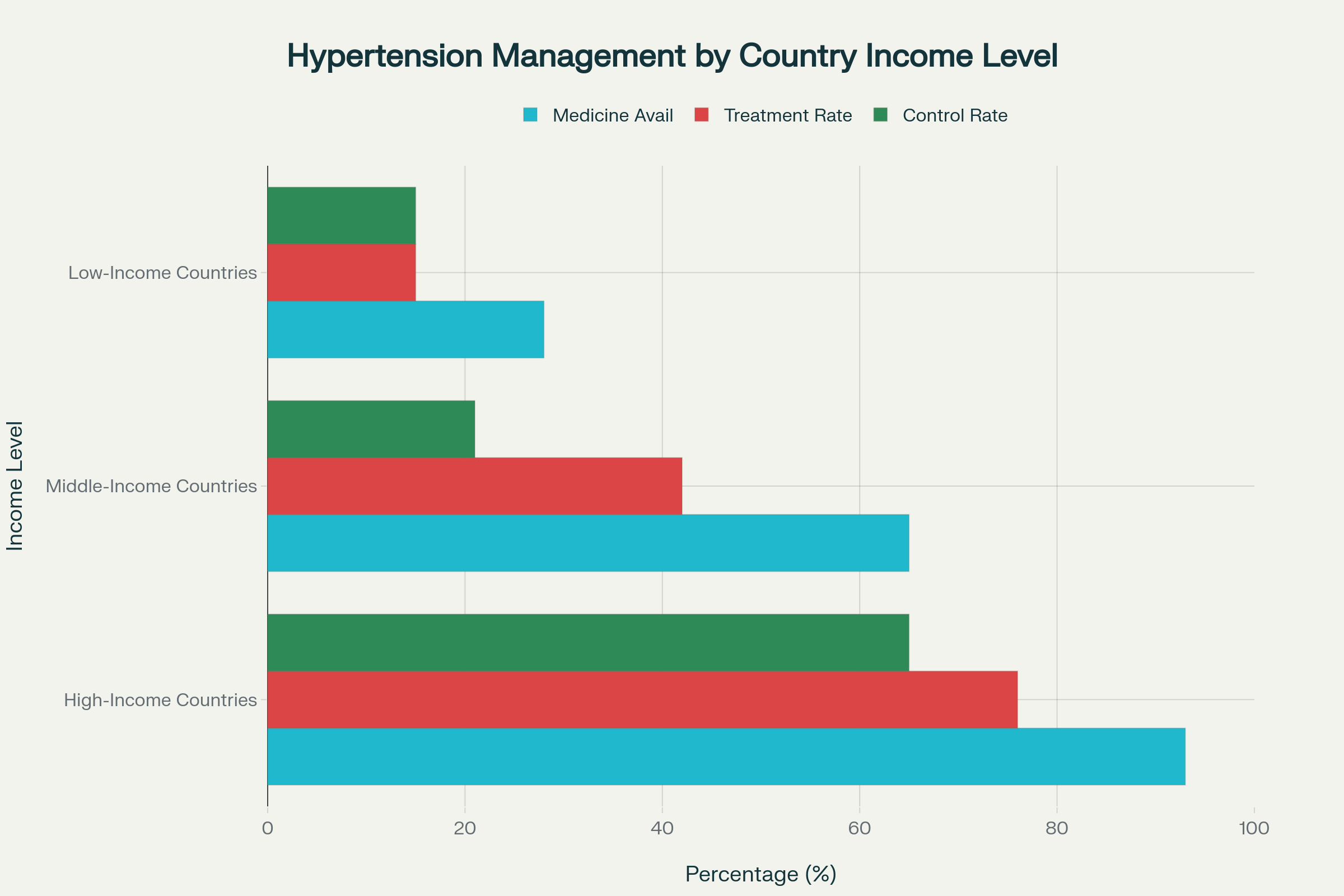
Hypertension management varies dramatically across income levels, with low-income countries facing severe treatment gaps
WHO Director-General Dr. Tedros Adhanom Ghebreyesus emphasized the preventable nature of deaths in this health crisis, stating that “every hour, over 1000 lives are lost to strokes and heart attacks from high blood pressure, and most of these deaths are preventable”. The global hypertension crisis has evolved into a leading cause of heart attack, stroke, chronic kidney disease, and dementia worldwide. Research indicates that this condition contributed to 10.7 million deaths in 2015 alone, representing 19.2% of all global deaths. Countries addressing the global hypertension crisis through integrated universal health coverage have demonstrated significant progress in reducing mortality rates.
No other risk factor claims as many lives as #hypertension.
— Tedros Adhanom Ghebreyesus (@DrTedros) September 23, 2025
But only around 1 in 5 people with hypertension have it under control.
The biggest barrier is access to medicines and affordable, validated blood pressure devices.
If we can control hypertension in just half of those… pic.twitter.com/j83XX0Ktc7
Economic Burden Threatens Global Development Goals
- US$3.7 trillion projected cost to low and middle-income countries from cardiovascular diseases between 2011-2025
- Economic impact represents approximately 2% of combined GDP for affected nations
- 31% of households in low-income countries cannot afford two basic blood pressure-lowering medicines
The financial implications of the global hypertension crisis extend far beyond healthcare systems, threatening economic stability across developing nations. Cardiovascular diseases stemming from this health emergency are projected to cost low and middle-income countries approximately US$3.7 trillion between 2011 and 2025, equivalent to roughly 2% of their combined gross domestic product. This massive economic burden diverts resources from education, infrastructure, and other development priorities. The global hypertension crisis creates a vicious cycle where countries least able to afford treatment face the highest disease burdens and economic losses.
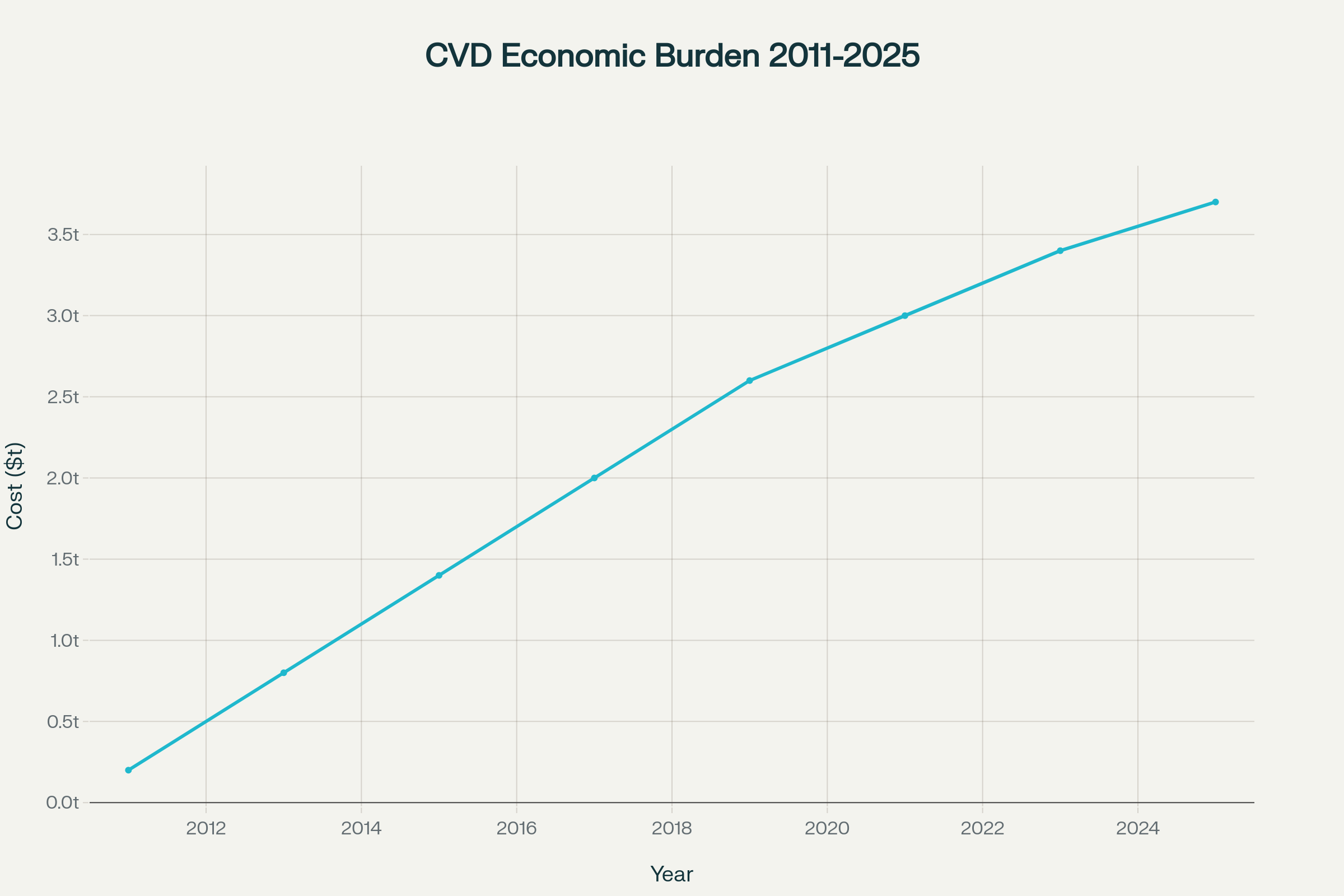
Economic burden of cardiovascular diseases projected to reach $3.7 trillion by 2025 in developing nations
Medicine accessibility remains a critical barrier in addressing the global hypertension crisis, with stark disparities between income levels. Research demonstrates that 31% of households in low-income countries cannot afford two blood pressure-lowering medicines, compared to 9% in middle-income countries and less than 1% in high-income nations. This health emergency perpetuates these inequalities as only 28% of low-income countries report general availability of all WHO-recommended hypertension medicines in pharmacies or primary care facilities. Communities lacking access to affordable medications show significantly lower rates of blood pressure control, directly contributing to this ongoing crisis.
The availability of multiple drug classes varies dramatically across economic regions, further complicating efforts to address the global hypertension crisis. High-income countries maintain 94% availability of four drug classes in communities, while this drops to 13% in low-income countries, highlighting systemic failures in the response. Dr. Tom Frieden, President and CEO of Resolve to Save Lives, noted that “safe, effective, low-cost medicines exist, but they are still out of reach for too many” people affected by this condition. These accessibility challenges transform the global hypertension crisis from a medical issue into a broader social justice concern.
Regional Variations Reveal Success Stories and Challenges
- Bangladesh increased hypertension control from 15% to 56% in some regions between 2019-2025
- Republic of Korea achieved 59% national blood pressure control rate in 2022 through integrated health reforms
- Philippines successfully incorporated WHO’s HEARTS technical package into nationwide community-level services
Geographic analysis of the global hypertension crisis reveals significant variations in prevalence, treatment, and control rates across different regions. Countries like Paraguay lead in hypertension prevalence with 62% of men and 51% of women affected, while others demonstrate that this condition can be effectively managed through proper policies. The WHO Western Pacific and Southeast Asia regions experienced a 144% increase in hypertension cases over thirty years, representing the fastest-growing epicenters of this health emergency. These regional patterns highlight how the condition affects different populations based on genetic, environmental, and healthcare system factors.
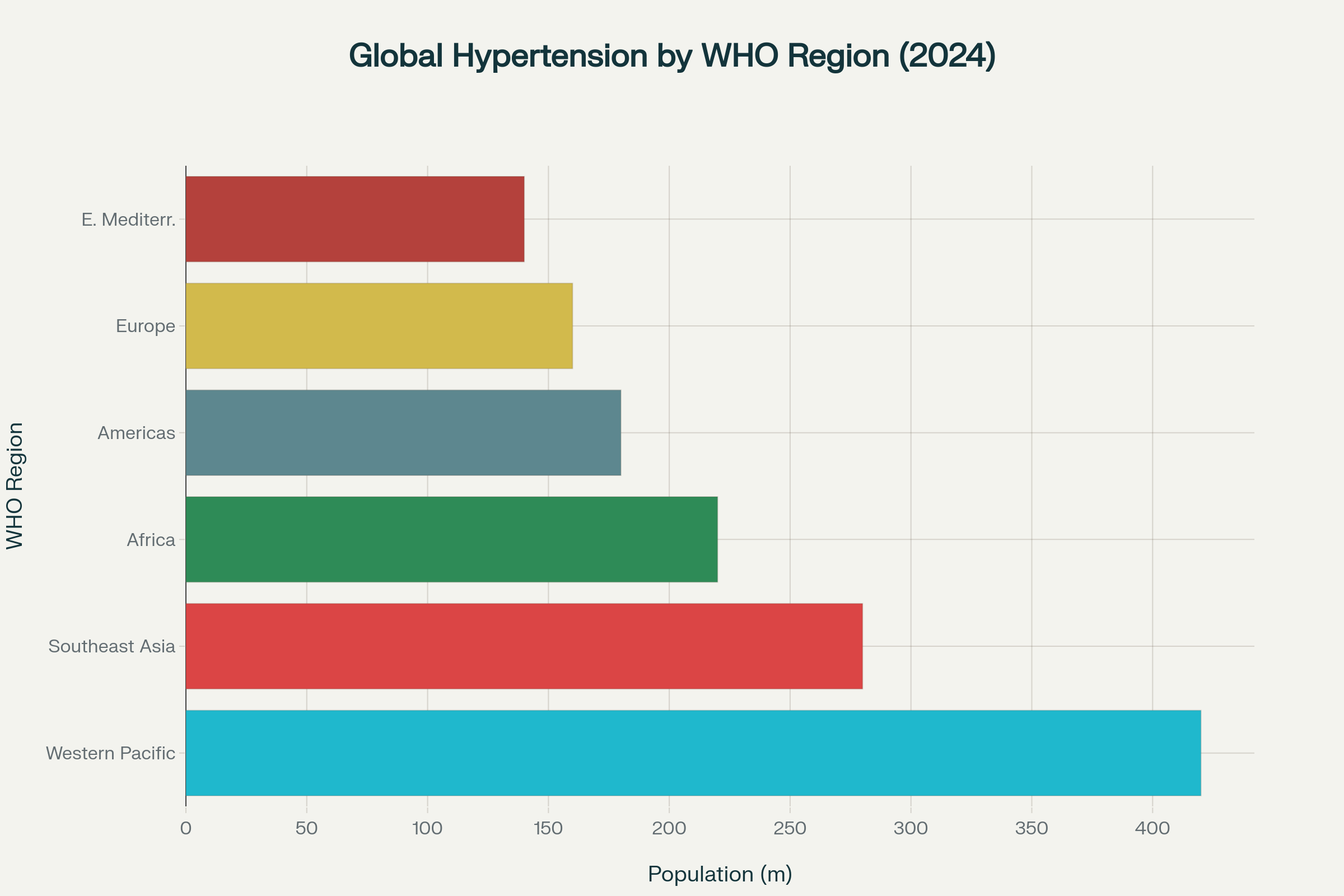
Western Pacific and Southeast Asia regions bear the highest hypertension burden globally
Success stories in managing the global hypertension crisis provide blueprints for global expansion. Bangladesh’s remarkable progress demonstrates how integrating hypertension treatment into essential health service packages can dramatically improve outcomes. The country increased hypertension control from 15% to 56% in targeted regions by strengthening screening and follow-up care within their universal health coverage framework. South Korea’s approach through low medication costs and limited patient fees resulted in 59% national blood pressure control by 2022.
Treatment rates also vary significantly, with Canada achieving 76% treatment rates for men with hypertension while countries like Rwanda manage only 10%. This health condition affects women and men differently across regions, with treatment disparities reflecting broader healthcare access inequalities. Countries successfully addressing the global hypertension crisis typically combine strong primary care systems, affordable medications, and comprehensive screening programs. The Philippines’ nationwide implementation of WHO’s HEARTS technical package demonstrates how systematic approaches can scale effective interventions across entire countries battling this condition.
Healthcare System Barriers Perpetuate Crisis
- Weak health promotion policies on tobacco, alcohol, and salt intake contribute to poor prevention
- Limited access to validated blood pressure monitoring devices hampers early detection
- Insufficient training of primary care personnel reduces treatment quality and continuity
Systemic healthcare weaknesses amplify the global hypertension crisis by creating multiple barriers to effective prevention, detection, and treatment. Analysis reveals that weak health promotion policies addressing risk factors like tobacco use, alcohol consumption, and excessive salt intake contribute significantly to this health emergency. Poor access to validated diagnostic tools means many cases remain undetected until complications arise. The absence of standardized treatment protocols creates inconsistent care quality, allowing this condition to persist even where resources exist.
Primary care system deficiencies represent critical bottlenecks in addressing the global hypertension crisis effectively. Insufficiently trained primary care personnel struggle to manage the complex needs of patients affected by this condition. Fragile supply chains for essential medications mean that even diagnosed patients cannot consistently access treatments needed to control their blood pressure. These interconnected system failures create a cascade effect where individual barriers compound to maintain this health emergency at population levels.

The WHO’s HEARTS technical package offers a comprehensive framework for countries seeking to address the global hypertension crisis through systematic healthcare improvements. This evidence-based approach provides practical modules covering treatment protocols, medicine access, risk-based management, and quality improvement systems. Countries implementing HEARTS components show measurable progress in reducing the impact through improved detection, treatment, and control rates. The technical package has supported 38 countries in treating 22.9 million patients worldwide by 2024, demonstrating scalable solutions for this health challenge.
Closing Assessment: Urgent Action Required
The global hypertension crisis stands as one of the most solvable yet persistent health challenges of our time, demanding immediate coordinated international action. With 1.4 billion people affected worldwide and only one in five achieving proper control, this represents a massive failure of global health systems to deliver basic, life-saving care. The projected US$3.7 trillion economic burden on developing nations over the next decade transforms this from a health issue into an urgent development priority requiring international cooperation and resource mobilization.
Success stories from Bangladesh, South Korea, and the Philippines prove that the global hypertension crisis can be effectively addressed through political will, sustained investment, and systematic healthcare reforms. Countries must embed hypertension control within universal health coverage frameworks while ensuring affordable access to essential medicines and trained healthcare personnel. This health emergency will continue claiming over 10 million lives annually unless nations implement comprehensive strategies addressing prevention, detection, treatment, and long-term management simultaneously. The tools to end the global hypertension crisis exist today, but their deployment requires unprecedented global commitment to health equity and universal access to essential care.