Key Highlights
- Research breakthrough: Southern California study reveals 18% of urinary tract infections stem from contaminated meat and poor kitchen hygiene practices, not just bathroom habits
- Poultry poses highest risk: Turkey shows 82% E. coli contamination rate, chicken 58%, while beef records 47% contamination in retail samples
- Socioeconomic disparity: Low-income communities face 60% higher risk of foodborne UTIs compared to affluent neighborhoods
Opening Overview
A groundbreaking study from Southern California has fundamentally shifted our understanding of urinary tract infection prevention, revealing that nearly one in five UTI cases may originate from contaminated meat and inadequate kitchen contamination UTI protocols rather than traditional bathroom-related causes. This revolutionary research, published in mBio journal, analyzed over 5,700 E. coli samples from UTI patients and compared their genetic fingerprints with contaminated meat samples from neighborhood grocery stores between 2017 and 2021.
The findings expose a critical food safety gap where kitchen contamination UTI transmission occurs through cross-contamination pathways previously overlooked by healthcare professionals. For countries like India, where UTI prevalence reaches 33.54% according to clinical studies, this research demands immediate attention to kitchen contamination UTI prevention protocols alongside traditional methods.
1 in 5 UTIs Can Be Linked to Poor Hygiene in The Kitchen… pic.twitter.com/JqcLtxdgdZ
— Katherine Stiles (@_K_Stiles) October 29, 2025
Scientific Evidence Behind Foodborne UTI Transmission
- Comprehensive genetic analysis reveals 18% of UTI-causing E. coli strains match animal-derived bacteria found in retail meat samples
- Multi-year surveillance tracked infection patterns across Southern California neighborhoods from 2017 to 2021
The research team from George Washington University and Kaiser Permanente Southern California conducted molecular analysis of more than 12,616 E. coli isolates from retail meat and 23,483 from UTI patients, creating the largest comparative study of its kind. Scientists used advanced genomic sequencing to establish direct genetic links between extraintestinal pathogenic E. coli (ExPEC) strains causing UTIs and identical bacterial populations found in commercially available meat products.
This foodborne kitchen contamination UTI connection challenges decades of medical assumptions that focused primarily on personal hygiene and sexual activity as primary transmission routes. The study’s methodology eliminated coincidental similarities by matching bacterial strains from UTI patients with meat samples purchased from stores in their specific neighborhoods, establishing clear geographical and temporal kitchen contamination UTI connections.
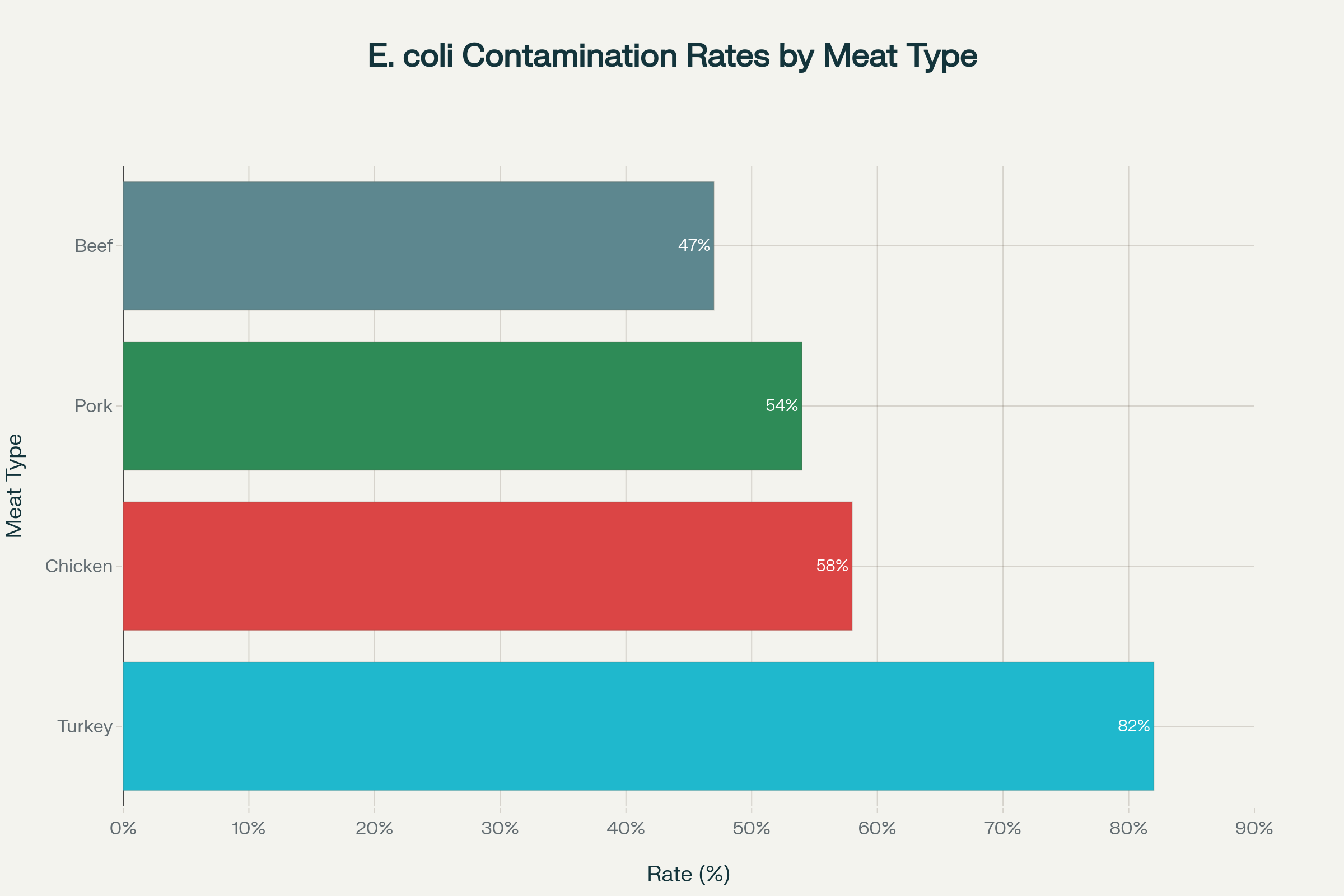
E. coli contamination rates vary significantly across different meat types, with poultry showing the highest contamination levels
According to the Centers for Disease Control and Prevention, proper food safety protocols can prevent most kitchen-based bacterial transmission, emphasizing hand washing for at least 20 seconds after handling raw meat and maintaining separate cutting boards for different food types. The World Health Organization estimates that contaminated food causes 600 million illnesses globally each year, with bacterial infections representing a significant portion of this disease burden. Research data shows that UTI recurrence rates in India range from 22.30% in population studies, suggesting that addressing kitchen contamination UTI pathways could substantially reduce this health burden.
Contamination Patterns Across Different Meat Categories
- Poultry products demonstrate highest contamination rates with turkey at 82% and chicken at 58% E. coli presence
- Red meat contamination varies significantly between pork (54%) and beef (47%) in retail samples
The comprehensive contamination analysis reveals stark differences in bacterial presence across meat categories, with poultry products showing consistently higher E. coli contamination rates compared to red meat alternatives. Turkey samples demonstrated the highest contamination levels at 82%, followed closely by chicken at 58%, indicating that poultry processing and handling protocols require immediate industry attention for kitchen contamination UTI prevention.
Pork products showed moderate contamination at 54%, while beef recorded the lowest rates at 47%, though all categories exceeded safe consumption thresholds without proper cooking procedures. The study identified that contamination was particularly prevalent in ‘value pack’ meat products, which contain larger quantities sold at lower per-pound prices, potentially indicating compromised handling during bulk processing that increases kitchen contamination UTI risks.
| Meat Type | E. coli Contamination Rate | UTI Link Strength | Risk Category |
|---|---|---|---|
| Turkey | 82% | Highest | Critical |
| Chicken | 58% | High | Severe |
| Pork | 54% | Moderate | Significant |
| Beef | 47% | Lower | Moderate |
Source: Southern California UTI-Meat Contamination Study, 2017-2021
Research indicates that industrialized farming practices may contribute to higher bacterial loads in meat products, with antibiotic-resistant E. coli strains becoming increasingly common in food production systems. The CDC’s food safety guidelines emphasize cooking poultry to internal temperatures of 165°F and ground meats to 160°F to eliminate harmful bacterial populations that cause kitchen contamination UTI transmission. Indian food safety data from the Food Safety and Standards Authority reveals significant contamination concerns across the domestic food supply chain, with regulatory testing showing variable compliance rates across different states.
Socioeconomic Factors Amplifying UTI Risk Distribution
- Geographic health disparities show 60% higher foodborne UTI rates in low-income ZIP codes compared to affluent areas
- Economic barriers limit access to quality meat products and proper food safety education in vulnerable communities
The study uncovered troubling socioeconomic patterns where residents of low-income neighborhoods experienced disproportionately higher rates of foodborne UTIs, with a 60% increased risk compared to residents of more affluent areas. This disparity reflects broader healthcare inequities where economic constraints force families to purchase lower-quality meat products, often sold in bulk packaging with higher kitchen contamination UTI risks. Research author Lance Price emphasized that “your risk of infection should not depend on your ZIP code,” highlighting systemic food safety failures that disproportionately affect vulnerable populations. The correlation between poverty and kitchen contamination UTI risk extends beyond individual purchasing decisions to include inadequate kitchen facilities, limited access to food safety education, and weaker regulatory enforcement in lower-income commercial districts.
Women showed higher susceptibility to foodborne UTIs compared to men, consistent with traditional UTI epidemiology patterns, though the specific mechanisms driving this gender disparity in food-related infections require further investigation. Indian UTI prevalence studies confirm that females account for approximately 66.78% of all UTI cases, with middle-aged women showing particularly high infection rates from kitchen contamination UTI sources. The intersection of gender, economic status, and food safety creates compound risk factors that demand targeted intervention strategies addressing both individual behavior modification and structural food system improvements. Public health experts argue that reducing foodborne UTI disparities requires comprehensive approaches including improved meat safety regulations, enhanced community food safety education, and economic policies that ensure equitable access to safe food products.
Kitchen Hygiene Protocols for UTI Prevention
- Cross-contamination prevention requires dedicated cutting boards, immediate surface sanitization, and proper hand hygiene protocols
- Temperature control demands internal cooking temperatures of 165°F for poultry and 160°F for ground meats to eliminate bacterial threats
Implementing effective kitchen hygiene protocols represents the most practical approach for reducing kitchen contamination UTI transmission in domestic settings. The CDC recommends washing hands for at least 20 seconds with soap and warm water before, during, and after food preparation, with particular emphasis on handwashing after handling raw meat products. Proper surface management requires using hot, soapy water followed by disinfectant solutions on all cutting boards, countertops, and utensils that contact raw meat, preventing bacterial reservoir formation that can persist for extended periods and cause kitchen contamination UTI incidents. Cross-contamination prevention demands strict separation of raw meat from ready-to-eat foods throughout the entire food preparation process, including separate cutting boards, utensils, and storage containers.
| Prevention Strategy | Implementation | Effectiveness Rating |
|---|---|---|
| Dedicated cutting boards | Raw meat only | High |
| 20-second hand washing | After each meat contact | Critical |
| Surface disinfection | Hot soapy water + sanitizer | High |
| Temperature monitoring | Food thermometer use | Essential |
| Proper storage | Sealed containers, bottom shelf | Moderate |
Source: CDC Food Safety Guidelines and UTI Prevention Protocols
Food thermometer usage ensures that internal temperatures reach levels sufficient to eliminate E. coli and other pathogenic bacteria, with poultry requiring 165°F and ground meats needing 160°F for safe consumption and kitchen contamination UTI prevention. Storage protocols emphasize keeping raw meat in sealed containers on the refrigerator’s bottom shelf to prevent dripping onto other foods, while maintaining refrigerator temperatures at 40°F or below. Indian households should pay particular attention to these protocols given the country’s warm climate and variable cold chain infrastructure, which can accelerate bacterial growth in improperly stored meat products and increase kitchen contamination UTI risks. Regular replacement of kitchen sponges and dishcloths prevents these items from becoming bacterial reservoirs that can recontaminate clean surfaces.
Final Assessment
The Southern California study fundamentally transforms our understanding of UTI prevention by establishing kitchen contamination UTI protocols as equally important to traditional bathroom-focused interventions. With 18% of UTI cases potentially linked to contaminated meat and poor food handling practices, healthcare providers must expand prevention counseling beyond personal hygiene to include comprehensive kitchen contamination UTI education.
The disproportionate impact on low-income communities demands systemic interventions addressing both individual behavior modification and structural improvements to food safety systems. For countries like India, where UTI prevalence exceeds 33%, integrating kitchen contamination UTI protocols into public health campaigns could significantly reduce infection rates and healthcare costs. This research represents a paradigm shift requiring coordinated responses from healthcare providers, food safety regulators, and community health educators to address this previously unrecognized kitchen contamination UTI transmission pathway.


