Key Highlights:
- Australian scientists create world’s first fully functioning lab-grown human skin with complete blood supply at University of Queensland
- Revolutionary lab-grown human skin includes hair follicles, blood vessels, nerves, immune cells, and tissue layers mimicking natural skin
- Breakthrough promises improved treatments for chronic skin diseases affecting 1.8 billion people worldwide
Opening Overview
Scientists at the University of Queensland have achieved a groundbreaking milestone in regenerative medicine by successfully growing the world’s first fully functioning lab-grown human skin complete with its own blood supply. This revolutionary advancement represents a major leap forward in tissue engineering, offering unprecedented hope for millions of patients suffering from severe skin diseases, burns, and genetic disorders. The lab-grown human skin model, developed over six years of intensive research, replicates natural human skin with remarkable precision, including blood vessels, capillaries, hair follicles, nerves, tissue layers, and immune cells.
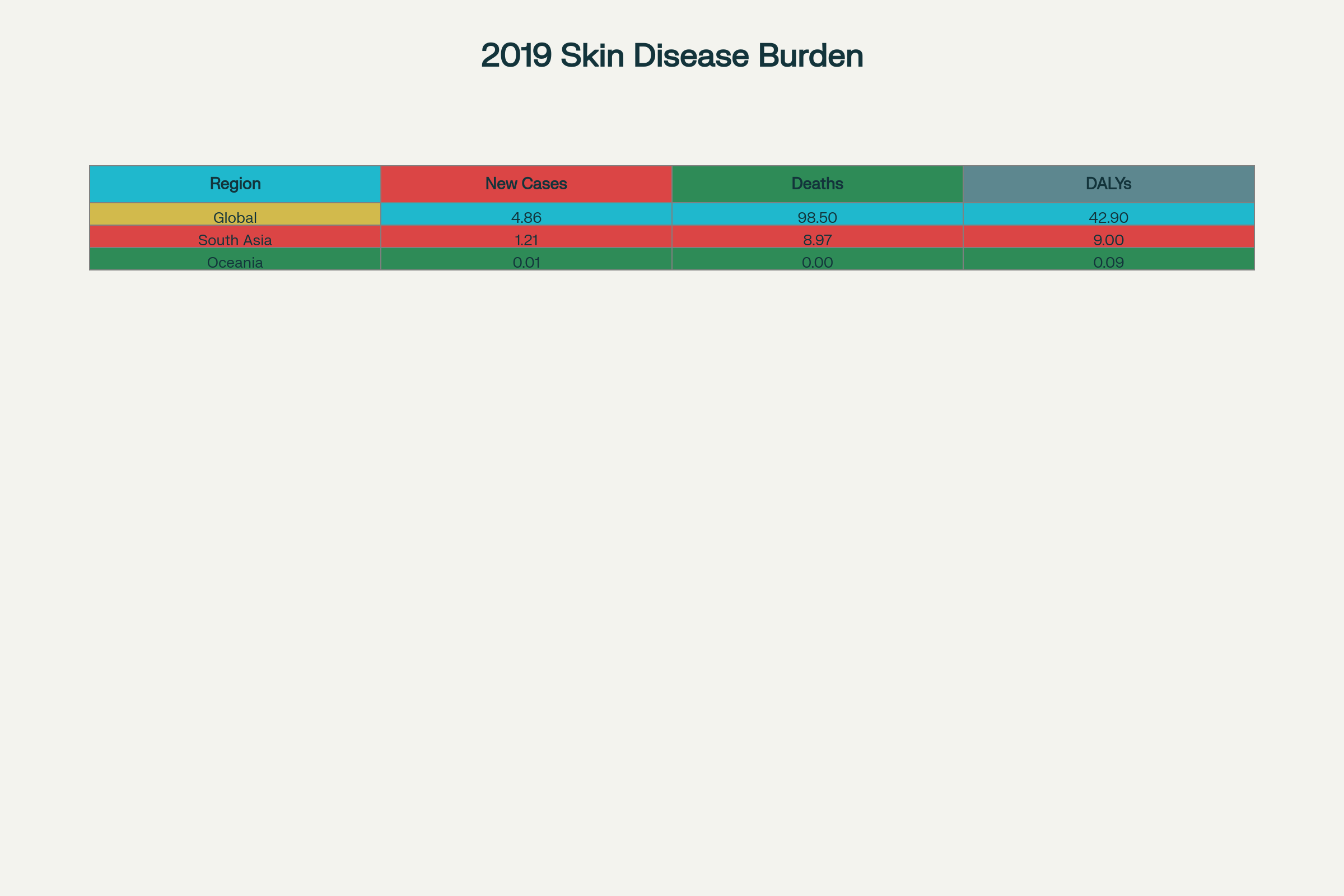
The significance of this lab-grown human skin breakthrough cannot be overstated, particularly given the global burden of skin diseases. According to World Health Organization data, skin conditions affect approximately 1.8 billion people at any given time, with the burden of skin and subcutaneous diseases measured at 42.9 million Disability-Adjusted Life Years in 2019. This lab-grown human skin technology promises to transform how researchers study skin diseases and develop new treatments, potentially revolutionizing care for patients with conditions ranging from severe burns to chronic inflammatory disorders.
Breakthrough in Lab-Grown Human Skin: A New Era for Skin Disease Treatment
- First fully functioning lab-grown human skin with blood supply developed
- Skin model replicates real human skin structures like hair follicles, blood vessels, and nerves
- Potential for better disease study and treatment innovation
Lead researcher Dr. Abbas Shafiee from UQ’s Frazer Institute emphasized the revolutionary nature of their lab-grown human skin development, stating it represents “the most life-like skin model that’s been developed anywhere in the world”. This lab-grown human skin breakthrough addresses critical limitations that have long hindered skin disease research and treatment development. Previous skin substitutes could not adequately replicate the complex architecture and functionality of natural human skin, making it difficult for researchers to study disease mechanisms or test potential therapies effectively.
The lab-grown human skin model incorporates all essential components found in natural skin, including sebaceous and sweat glands that previous models lacked. This comprehensive approach to creating lab-grown human skin ensures that researchers can study skin diseases in an environment that closely mirrors real human conditions. The tissue’s ability to develop pigmentation and appendage patterning further enhances its utility as a research tool, providing scientists with an unprecedented platform to understand how various skin conditions develop and progress.
The development process for this lab-grown human skin required extensive optimization of stem cell differentiation protocols. Researchers tested various stem cell lines and procedures to achieve optimal growth of skin organoids, which are three-dimensional skin tissues created in laboratory conditions. The resulting lab-grown human skin demonstrates remarkable similarity to natural tissue, positioning it as a game-changing tool for advancing dermatological research and therapeutic development.
Innovative Use of Stem Cells in Creating Lab-Grown Human Skin
- Human skin cells reprogrammed into stem cells to grow skin organoids
- Skin organoids include tissue layers, pigmentation, and immune cells
- Stem cell technology advances enable more life-like skin models
The creation of this lab-grown human skin relies on cutting-edge stem cell technology that begins with reprogramming human skin cells into induced pluripotent stem cells. These versatile stem cells can be transformed into any type of cell in the human body, providing the foundation for growing complex tissue structures. The research team placed these stem cells in petri dishes, where they underwent a carefully controlled four-month differentiation process to produce skin organoids that would eventually become fully functional lab-grown human skin.
A critical innovation in this lab-grown human skin development was the integration of a functional blood supply system. Researchers used the same stem cells to create tiny blood vessels, which were then added to the growing skin tissue. This vascular integration allowed the lab-grown human skin to develop just like natural human skin, with proper nutrient delivery and waste removal systems that are essential for tissue viability and function.
The stem cell-based approach to creating lab-grown human skin represents a significant advancement over previous tissue engineering methods. Earlier attempts to create skin substitutes often lacked the complexity and functionality needed for meaningful research applications. By utilizing induced pluripotent stem cells, the Queensland team successfully recreated the intricate cellular interactions and tissue architecture that characterize natural human skin, resulting in lab-grown human skin that can serve as an accurate model for disease study and treatment testing.
Implications of Lab-Grown Human Skin for Skin Disease Patients
- Improved grafts and treatment options for inflammatory and genetic skin disorders
- Chronic skin conditions like psoriasis, atopic dermatitis, and scleroderma can benefit
- Skin model enables more accurate testing of treatments and therapies
The development of lab-grown human skin holds tremendous promise for patients suffering from various inflammatory and genetic skin disorders. Professor Kiarash Khosrotehrani from UQ’s Frazer Institute highlighted that this lab-grown human skin technology could significantly improve grafts and treatments for conditions such as psoriasis, atopic dermatitis, and scleroderma. These chronic conditions often prove resistant to conventional therapies, leaving patients with limited treatment options and reduced quality of life.
Current stem cell therapies have already shown promising results in treating autoimmune and inflammatory skin diseases, with mesenchymal stem cells demonstrating beneficial outcomes in conditions unresponsive to conventional therapy. The availability of lab-grown human skin models could accelerate the development of more effective treatments by providing researchers with accurate platforms to test new therapeutic approaches. This lab-grown human skin technology enables scientists to study disease mechanisms more closely and evaluate potential treatments before progressing to human clinical trials.
For burn victims and patients requiring skin grafts, lab-grown human skin technology offers the potential for dramatically improved outcomes. Traditional skin grafts often result in scarring and irritation at wound sites, but lab-grown human skin could provide grafts that look and function more like the patient’s natural skin. This advancement could transform the treatment landscape for severe burn injuries, potentially reducing patient suffering and improving long-term recovery outcomes.
Global Skin Disease Burden and the Role of Lab-Grown Skin in Future Therapies
- Skin diseases affect over 1.8 billion people worldwide
- Growing global burden with significant impact in low to middle income countries
- Lab-grown skin could revolutionize treatment and reduce disability
The global burden of skin and subcutaneous diseases presents a significant public health challenge, with official data indicating that these conditions accounted for 42.9 million Disability-Adjusted Life Years in 2019. The development of lab-grown human skin technology comes at a critical time when skin disease prevalence continues to rise globally, particularly in low to middle-income countries where access to advanced treatments remains limited.
Regional disparities in skin disease burden highlight the urgent need for innovative solutions like lab-grown human skin technology. South Asia reported the highest number of new skin disease cases and deaths in 2019, with over 1.2 billion new cases recorded. Western Sub-Saharan Africa showed the most significant percentage increase in cases and disability-adjusted life years, rising by 137% and 140% respectively from 1990 to 2019. These statistics underscore the potential impact that lab-grown human skin technology could have on global health outcomes.
The WHO has recognized skin diseases as a global public health priority, noting that skin conditions affect approximately 1.8 billion people at any point in time. Fungal infections represent the largest category of skin diseases globally, accounting for 34% of new cases, followed by bacterial skin diseases at 23%. The availability of lab-grown human skin models could accelerate research into treatments for these common conditions, potentially reducing the global disease burden and improving quality of life for millions of patients worldwide.
Closing Assessment
The successful development of the world’s first fully functioning lab-grown human skin with its own blood supply represents a watershed moment in regenerative medicine and dermatological research. This groundbreaking achievement by University of Queensland scientists offers tangible hope for the millions of people worldwide suffering from skin diseases, burns, and genetic disorders. The lab-grown human skin model’s ability to accurately replicate natural human skin architecture and function provides researchers with unprecedented opportunities to study disease mechanisms and test potential treatments.
As the global burden of skin diseases continues to grow, affecting 1.8 billion people worldwide with significant impacts on quality of life and healthcare systems, the timing of this lab-grown human skin breakthrough could not be more critical. The technology promises to accelerate the development of more effective treatments while potentially reducing the need for traditional skin grafts and their associated complications. While the transition from laboratory success to clinical application will require additional research and regulatory approval, this lab-grown human skin advancement marks a significant step toward a future where severe skin conditions no longer represent insurmountable medical challenges.


