Summary
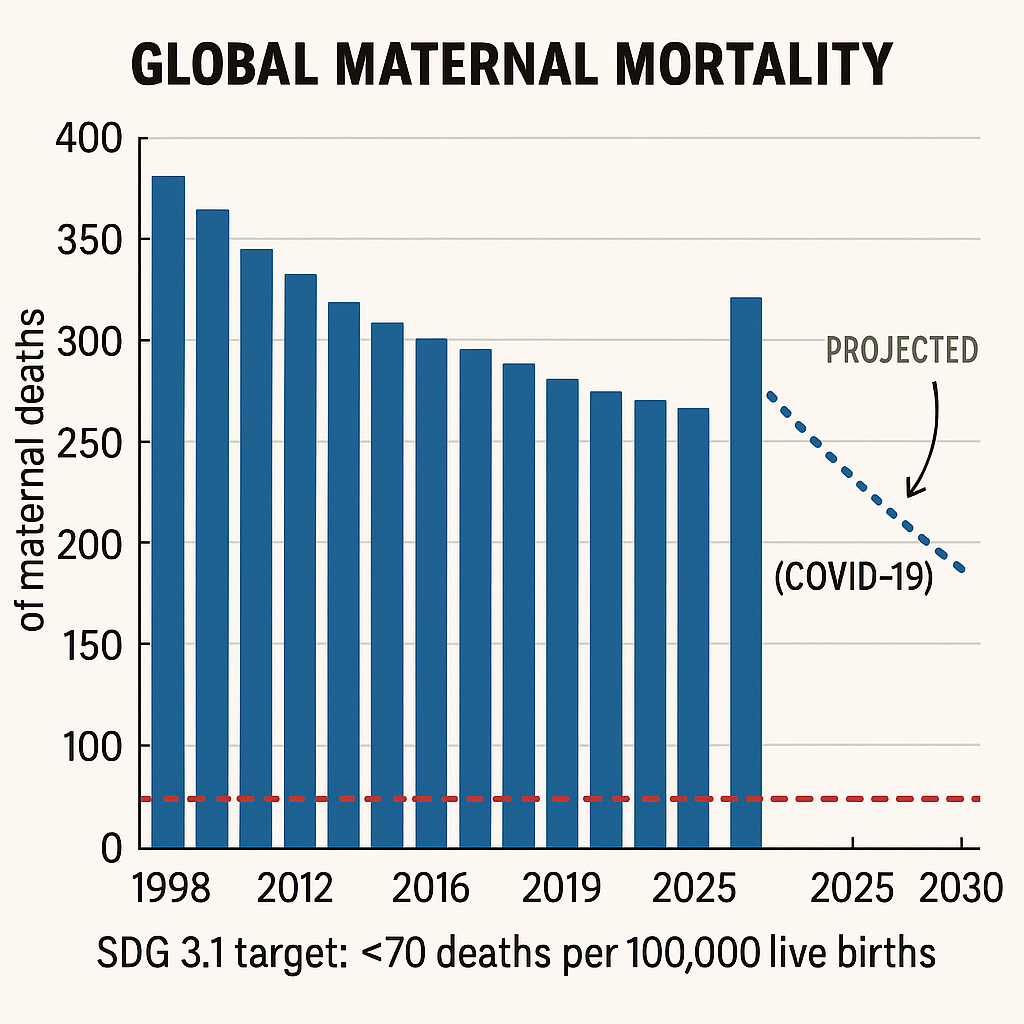
- A new UN report warns that the aid cuts maternal mortality 2025 crisis could erase a 40 % drop in maternal deaths since 2000, with 260,000 women already lost in 2023—one every two minutes.
- The U.S. freeze on USAID health grants and Britain’s reduced overseas budgets are shutting clinics, slashing midwife posts and stalling hemorrhage-control supply chains in 38 low-income countries.
- Knock-on effects—malaria, HIV, WFP nutrition cuts—amplify the aid cuts maternal mortality 2025 toll, with Ethiopia alone suspending treatment for 650,000 women and children.
Fiscal Fault-Lines: Why the Money Gap Now Kills More Than the Medicines Ever Saved
Between 2000 and 2023, coordinated global investment built a fragile safety net: skilled-birth attendance rose from 62 % to 83 %, antenatal care quadrupled in parts of sub-Saharan Africa, and maternal deaths plunged by nearly half. That progress, the UN says, is now “experiencing a pandemic-like shock without the virus”—because aid cuts maternal mortality 2025 have yanked away the very financing that underwrote those gains.
Yet budget lines fade faster than trust is built. Midwives trained on donor dollars are receiving dismissal notices; rural clinics stand dark as diesel for generators dries up; and procurement orders for magnesium sulphate, a cheap lifesaver for pre-eclampsia, languish in unfunded spreadsheets. In many capitals, local treasuries—stretched by climate disasters and debt service—cannot fill the void. The result: an avoidable return to what WHO Director-General Tedros calls “the most dangerous journey a woman will ever undertake—childbirth in a broken system.”
When a mother dies in pregnancy or childbirth, her baby’s life is also at risk.
— Catherine Russell (@unicefchief) April 6, 2025
Global funding cuts to health services put more pregnant women at risk, especially in the most fragile settings, and threaten fragile progress in ending maternal deaths.👇 https://t.co/UPqmmMviBS
Pipeline to Peril: How Donor Retrenchment Reversed Two Decades of Momentum
- USAID’s global health spend faces a 44 % freeze, touching 30 maternal-health programs; parallel British ODA cuts removed £4 billion from 2025 baselines.
- UN tracking shows 70 % of halted projects are in fragile or conflict-hit states, exactly where maternal risk is highest.
- Forecast models estimate the aid cuts maternal mortality 2025 shock could add 60,000 deaths a year by 2027—wiping out SDG-aligned targets.
- Countries already backsliding before COVID-19—Venezuela, Jamaica, Dominican Republic, the United States—now face steeper climbs.
- Every US $1 billion withdrawn translates to 7,000 additional maternal fatalities, the UNFPA cost-curve shows.
The Domino Effect
Aid is rarely a single budget line: it underwrites supply chains, pays salary top-ups that keep midwives in rural posts, and finances referral ambulances. When Washington froze allocations in February, warehouse contracts lapsed by March, and magnesium sulphate stock-outs appeared by April in Honduras, Malawi and Nepal. The “fiscal frost” also chills co-financing deals: Norway paused a match-fund program for Sierra Leone’s blood banks, citing uncertainty over U.S. participation. Thus the aid cuts maternal mortality 2025 spiral feeds on itself—every donor’s retreat nudging another to follow.
Numbers in Reverse
On the Ward Floor: Voices from the Frontlines of a Fiscal Emergency
- Ethiopia’s WFP-run supplementary feeding halted for 650,000 mothers and infants, after donor inflows dried to a quarter of 2022 levels.
- In Sierra Leone’s Kailahun district, 12 of 17 maternity staff were laid off when a USAID payroll grant expired in March.
- Ugandan obstetric wards report hemorrhage case-fatality rates doubling as uterotonics run short due to shipping disruptions.
- Malaria drug shortages heighten maternal risk: 20 % of pregnancy-related deaths in West Africa link to untreated malaria.
- Midwife “brain drain” accelerates—richer neighbours lure unpaid staff, worsening aid cuts maternal mortality 2025 hotspots.
Testimony of Attrition
At Yirgalem General Hospital in southern Ethiopia, Dr. Selamawit Girma tracks cases of postpartum hemorrhage. In January she lost one woman a week; by March—after the nutrition program paused—she lost three. Malnourished mothers bleed more and clot less, she says. “You feel you’re drowning, and the lifeboat is being towed away.” Similar stories echo in Uganda’s Lira, Pakistan’s Balochistan and Haiti’s Artibonite. Each recounts a simple equation: fewer dollars, fewer drugs, more funerals—amplifying the aid cuts maternal mortality 2025 pattern.
The Compounders
Maternal survival is not isolated; it leans on HIV prophylaxis, malaria nets and cholera vaccines. Aid pull-backs in these vertical programs ripple into obstetrics. In Zimbabwe, a Global Fund funding gap cut antiretroviral coverage for pregnant women, sparking a rise in HIV-related obstetric sepsis. In Afghanistan, Talib restrictions plus donor fatigue shuttered 45 women-run health posts, forcing expectant mothers into risky home births. These intertwined crises mean the aid cuts maternal mortality 2025 story is larger than any maternity ward—it is a systemic unraveling.
Alternatives—or Illusions? Domestic Revenues, Philanthropy and Tech Fixes
- Some governments hike sin taxes (tobacco, alcohol) to fill the maternal-health void, but yields cover barely 20 % of lost aid.
- Philanthropic pledges surge online—yet 75 % target flashy digital apps, not unglamorous blood banks or surgical kits.
- Tele-midwifery pilots show promise: WhatsApp triage lines in Kenya cut referral delays by 30 %, cushioning the aid cuts maternal mortality 2025 shock locally.
- Domestic resource mobilisation faces headwinds—debt servicing in low-income countries averages 39 % of revenue, limiting fiscal space.
- Climate-linked disasters siphon budget from health to relief; Mozambique’s 2024 cyclone repairs consumed an entire year’s health-capital allocation.
Counting on Home Coffers
Finance ministers from Nepal to Nigeria insist they will “own our destiny,” yet their cash tills tell another tale. Nigeria’s oil earnings fell 14 % in Q1 2025; Ghana’s cocoa prices slid despite record harvests. Innovative taxes—mobile-money levies, airline-ticket surcharges—raise single-digit millions, a fraction of the hundreds of millions evaporating via aid cuts maternal mortality 2025. And without predictable disbursement, even small-scale community solutions struggle to plan.
Tech’s Limited Lifeline
Digital tools excite donors and VCs alike. But a smartphone video link cannot replace a transfusion if the blood fridge is empty. UNICEF’s small-pilot drone delivery in Malawi shaved hours off emergency kit delivery, yet scale-up costs eclipse current budgets. Technology can narrow the gap, not close it, underscoring that the aid cuts maternal mortality 2025 crisis is fundamentally fiscal, not merely logistical.
Last Chance Lifelines: Re-Funding the Future or Reopening Old Graves
The world knows how to save mothers. Skilled birth attendants, infection prevention, timely cesareans and respectful care cut deaths by up to 90 %. What the aid cuts maternal mortality 2025 saga reminds us is that knowledge without cash is ideology without impact. If wealthy nations retreat behind domestic walls, they gamble hard-won global credibility and consign thousands of women to avoidable graves.
Re-channeling dormant Special Drawing Rights, taxing windfall fossil profits, or ring-fencing a micro-levy on global financial flows—policy ideas abound. The harder task is political will. Maternal mortality rarely sways elections in donor nations, but it shapes demographic futures in recipient states. Bridging that empathy gap demands reframing aid not as charity but as insurance: a modest premium to avert the catastrophic loss of life and stability that unchecked maternal deaths unleash.
Fail to act, and the next decade’s obituary of progress will read: “She died because the line-item did.” Fund the lifelines, and childbirth can resume its rightful place as a moment of hope, not hazard. The ledger is open; what the world writes next will decide whether aid cuts maternal mortality 2025 becomes a short-lived scare—or the first chapter in a preventable regression.


